Have you got your sun protection? With summer almost upon us, the Cancer Council delivers a timely reminder about the dangers of too much UV exposure and explains what to look for when checking for the early signs of skin cancer.
Australia has one of the highest incidence rates of skin cancer in the world and it has risen over the past few decades. Two in three Australians will be diagnosed with skin cancer by the age of 70.
Skin cancer accounts for around 80 per cent of all newly diagnosed cancers and every year, Australian GPs have over one million patient consultations for skin cancer.
Although the statistics are scary, skin cancer is actually one of the most preventable cancers in Australia. Being SunSmart during both work and play is a key factor in reducing your risk.
Knowing how skin cancer occurs, what warning signs to look out for, and how to properly protect yourself will all arm you against becoming another statistic.
WHAT IS SKIN CANCER?
Cancer is a disease of the body’s cells. Normally, our cells grow and multiply in a controlled way.
Skin cancer occurs when something, for example overexposure to ultraviolet (UV) radiation from the sun, causes a ‘mistake’ to occur in the skin cells’ genetic blueprints. This can cause control to be lost and collections of these cells can grow and potentially spread within the body. ‘Cancer’ is the term used to describe this.
There are three main types of skin cancer, each named after the skin cell that the cancer resembles or develops from:
- Melanoma – the most dangerous form of skin cancer and the fourth most common cancer in Australia.
- Basal cell carcinoma (BCC) – making up about 70 per cent of non-melanoma skin cancers in Australia.
- Squamous cell carcinoma (SCC) – making up approximately 30 per cent of non-melanoma skin cancers in Australia.
Basal cell and squamous cell carcinomas are often grouped together and referred to as ‘common’ or ‘nonmelanoma’ skin cancers.
UV RADIATION AND YOUR SKIN
Anyone can be at risk of developing skin cancer, but risk increases with skin type and with age.
UV radiation, whether solar or artificial, is a major risk factor. Between 95 and 99 per cent of skin cancers in Australia result from excessive UV exposure and sunburn causes 95% of melanomas.
Some skin types are more sensitive to UV radiation and therefore burn more quickly. This means people with these skin types are at greater risk of skin cancer.
READ RELATED CONTENT
- New research says men are ignoring sun exposure
- Wearing the right sunglasses
- Sun safety | It’s time to get serious
Only people with naturally very dark skin (generally type V or VI) rarely, if ever, get burnt. Their skin has a larger amount of melanin which acts as a natural protection from UV radiation, lowering their risk of skin cancer. However, they should still take care when UV levels are high. Although people with very dark skin do not normally need to apply sunscreen, eye damage can occur in people of any skin type, so they should still wear hats or sunglasses.
WHAT TO LOOK OUT FOR
If found early, skin cancer can generally be treated successfully. However, it can be fatal if left untreated. Knowing your skin and recognising when there are changes can literally save your life.
In general, skin cancer stands out as being quite different to surrounding skin. It mostly appears as a new and unusual looking spot. However, it can also appear as an existing spot that has changed in colour, size or shape.
“Knowing how skin cancer occurs, what warning signs to look out for, and how to properly protect yourself will all arm you against becoming another statistic.”
NON-MELANOMA SKIN CANCER
Non-melanoma skin cancers often appear as crusty, non-healing sores or small lumps that are red, pale or pearly in colour. New spots, freckles, or any moles that change in colour, thickness or shape over a period of weeks to months (especially those that change from dark brown to black, red or blue-black in colour) are also symptomatic of non-melanoma skin cancer.
To diagnose a non-melanoma skin cancer, a small sample of tissue is removed for examination under a microscope. This is known as a biopsy. A biopsy is usually enough to determine the stage of the cancer.

MELANOMA
Melanoma is more often diagnosed in men than women. For men, the risk of being diagnosed by age 85 is 1 in 14 compared to 1 in 24 for women.
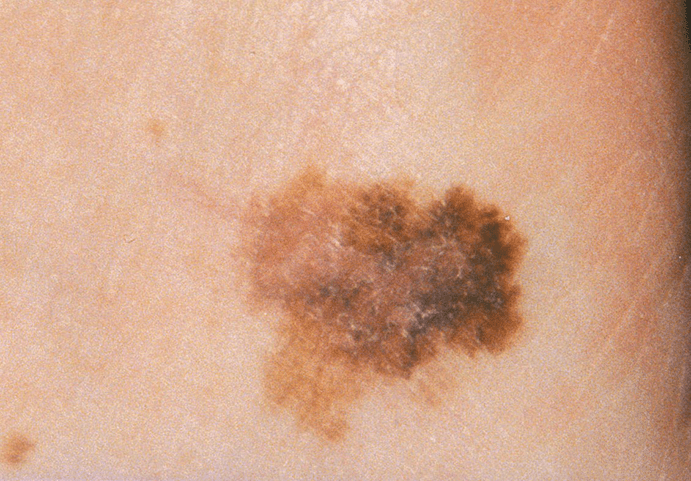
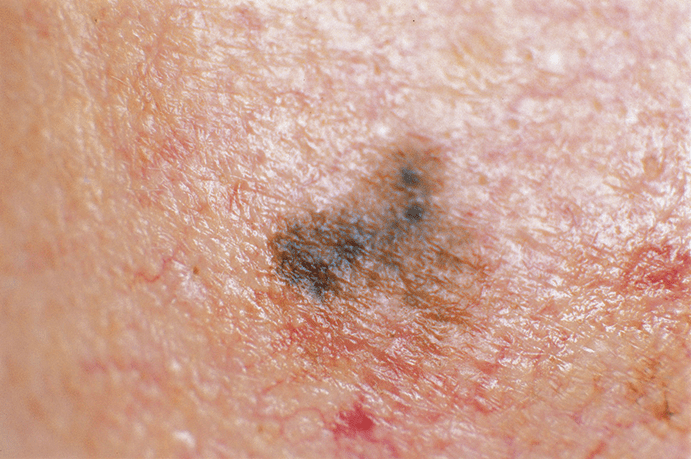
Melanoma often has no symptoms, however it can be associated with certain changes in the skin. The ‘ABCD’ of melanoma detection can be a useful guide when checking your skin.
- A is for Asymmetry – Look for spots that lack symmetry.
- B is for Border – A spot with a spreading or irregular edge (notched).
- C is for Colour – Blotchy spots with a number of colours such as black, blue, red, white and/or grey.
- D is for Diameter – Look for spots that are getting bigger.
HOW TO CHECK YOUR SKIN
Developing a regular habit of checking your skin will allow you to stay on top of any new spots or changes to existing freckles or moles. The earlier a skin cancer is identified and treated, the better your chance of avoiding surgery or, in the case of a serious melanoma or other skin cancer, potential disfigurement or even death.
- Make sure you check your entire body as skin cancers can sometimes occur in parts of the body not exposed to the sun; for example soles of the feet, between fingers and toes and under nails.
- Undress completely and make sure you have good light.
- Use a mirror to check hard to see spots, like your back and scalp, or get a family member, partner or friend to check for you.
Look out for changes such as:
- New moles.
- Moles that have increased in size.
- An outline of a mole that becomes notched.
- A spot that changes colour from brown to black or is varied.
- A spot that becomes raised or develops a lump within it.
- The surface of a mole becoming rough, scaly or ulcerated.
- Moles that itch or tingle.
- Moles that bleed or weep.
- Spots that look different from the others.
“…inappropriately designed and heavy covering clothing worn for sun protection purposes can contribute to an employee’s risk of heat illness.”
It can be difficult to know if something on your skin is a harmless mole, normal sun damage, or a sign of skin cancer. Though you might notice one or more skin changes, it does not necessarily mean you have skin cancer. Visit your GP when in doubt and have any moles/ skin changes investigated further.
PREVENTION OF SKIN CANCER
Australia has some of the highest UV levels in the world. On a fine day in January, UV radiation is intense enough to cause sunburn in just 11 minutes. Overexposure to UV is the major cause of sunburn, premature aging and eye damage.
UV cannot be seen or felt, unlike the sun’s light which we can see, or the sun’s warmth which we feel. Because our senses can’t detect UV, it can be damaging without us even realising it.
The SunSmart UV Alert is reported daily by the Bureau of Meteorology. It identifies times during the day when the UV level is 3 or above – times when sun protection is necessary. If there is no UV alert, sun protection is not needed unless you are near highly reflective surfaces such as snow.
For best protection, Cancer Council recommends a combination of sun protection measures, best summarised as ‘Slip, Slop, Slap, Seek and Slide’.
- Slip on some sun protective clothing that covers as much skin as possible. It is one of the best barriers between the skin and sun. Sun protective clothing includes long pants and collared, long sleeve shirts. Clothing with an Ultraviolet Protection Factor (UPF) rating of at least 15 is preferable. The higher the rating, the greater the protection provided by the fabric.
- Slop on some broad spectrum, water resistant SPF30+ (or higher) sunscreen. Apply it 20 minutes prior to heading outdoors and re-apply every two hours. Apply sunscreen liberally – at least a teaspoon for each limb, front and back of the body, and half a teaspoon for the face, neck and ears. If you do not apply enough, you will not receive the protection stated on the product.
- Slap on a broad-brimmed hat which will shade the face, ears and neck. Hats of this nature will also assist in protecting the eyes from UV radiation.
- Seek shade during peak UV radiation times.
- Slide on some sunglasses that meet Australian Standards. Cancer Council recommends wearing close-fitting, wraparound sunglasses as 40 per cent of UV reaching the eye can be attributed to peripheral light.
SUN SAFETY AT WORK
Outdoor workers receive five to ten times more UV exposure than indoor workers, increasing their risk of skin cancer.
Work health and safety legislation, specific to each Australian state and territory, requires employers to provide a safe working environment. This includes taking steps to reduce the known health risks associated with exposure to solar UV radiation for outdoor workers. It also requires workers to cooperate with a workplace’s sun protection program. This generally entails following any policies and procedures, attending training and following the instructions and advice provided, and using the supplied protective equipment as instructed.
HEAT ILLNESS
In addition to UV radiation, the sun emits other radiation including visible light (which we see) and infrared radiation (which we feel as heat).
Heat illness can occur when the body is unable to cope with working in the heat. The term covers a range of illnesses including heat stroke, heat exhaustion, heat cramps and skin rashes. Signs and symptoms of heat illness include nausea, dizziness, clumsiness, collapses and convulsions. If left untreated, heat illness can be fatal.
Although UV exposure and heat illness are separate occupational hazards for outdoor workers, the effects of heat must be considered when designing and implementing a sun protection program for the workplace. This is because working in the heat can contribute to non-compliance with sun protection measures if personal protective equipment and clothing is not used as intended due to heat discomfort. In addition, inappropriately designed and heavy covering clothing worn for sun protection purposes can contribute to an employee’s risk of heat illness. Materials and designs that provide sun protection while keeping workers cool in hot conditions should be selected.
Ultimately, when it comes to health in the workplace, prevention is far better than a cure. In consultation with health and safety representatives and employees, employers should identify solar UV exposure hazards and introduce control measures to reduce exposure.
Cancer Council Australia recommends that workplaces have a comprehensive sun protection program in place that includes:
- Risk assessment: periodic assessment of the solar UVR exposure risk to all employees.
- Sun protection control measures: the introduction and maintenance of protective measures in line with occupational hazard controls.
- Training employees to work safely in the sun: the provision of information, instruction, training and supervision for employees.
- Sun protection policy: documentation of the program, including control measures, in a written policy.
- Monitoring program effectiveness: a process to determine the effectiveness of control measures and identify changes that may further reduce exposure.
State and territory Cancer Councils may be able to assist workplaces with a sun protection policy, resources and strategies to create a sun safe working environment.
Although Australia has one of the highest rates of skin cancer in the world, being SunSmart is a simple and effective way to reduce your risk of developing skin cancer. Whether working indoors or outdoors, and regardless of skin type, no one need become another statistic.
PROFILE CANCER COUNCIL AUSTRALIA
Cancer Councils are the leading independent funders of cancer research in Australia, granting more than $54 million to cancer research, research scholarships and fellowships in 2013.
The Council provide evidence-based, up-to-date information about all aspects of cancer to:
- doctors and other health professionals – to help improve prevention, detection and treatment of cancer
- cancer patients and the general community – more than 100,000 Australians contact the Cancer Councils for information and advice each year, through the Cancer Council Helpline.
- Cancer Council Australia advises government on the needs of stakeholders and provides an independent voice for improved cancer control policy based on the evidence.
Cancer Council Australia also publishes the National Cancer Prevention Policy which advocates for a concerted and comprehensive national approach to the prevention of cancer. The policy makes specific recommendations for national action by governments and non-government organisations, including programs and strategies to reduce the incidence of cancer.














Add Comment